ICD-10 Impact and Strategies
For Criterions and TCMS Clients
Introduction
The mandated transition from ICD-9 to ICD-10 is October
1, 2014. The changes in coding and preparation are not optional and will vary
by the type of health care your office provides.
The ICD-10 transition is not a simple update of the
ICD-9 code set. The ICD-10 code sets have fundamental changes in structure and
concepts that make them very different from ICD-9. Because of these
differences, it is important to develop a preliminary understanding of the
changes from ICD-9 to ICD-10.
The goal of this document is to help clarify concerns of
the ICD10 transition and the use of our software.
Important Notes
Clearinghouses
Criterions will only test and support ICD-10
transmissions with Emdeon and with MedXpress.
Contents
CHAPTER 1 - Challenges in Coding
ICD-10 coding provides better data for analysis of
patterns related to disease and treatment outcomes. Claim submission processing
is projected to improve because claims become easier for the payers to
understand and gauge utilization.
Still, the journey towards these improvements leaves
little to no doubt that this transition will result in substantial coding
challenges due to significant changes in code structure, coding rules, code
detail, and the definition of codes. And, the most glaring change is in the
pure number of diagnosis codes now available: There are approximately14, 000
ICD-9 codes… there are about 68,000 ICD-10 codes.
Diagnosis coding has always represented a “necessary
evil” for most physicians. Codes are not used, for example, in communication
with a patient or their condition. But, it is an important task that ensures
payments. Coding is typically assigned to office staff that identifies the
correct codes from those stored in TCMS and uses them to submit claims to the
various payers. If there is an operational disconnect between the physician and
the coder, the quality of the coding suffers and results in inaccurate and
possibly unpaid claims.
Improved Coding Accuracy
It is important to avoid fearing that ICD-10 will cause
more trouble that it is worth. ICD-10 offers improvements over ICD-9 in
defining the patient’s condition. With a better alignment between physician documentation
and coding processes, the accuracy and efficiency of claim processing can be
greatly improved under ICD-10.
For example, ICD-9 codes today offer only one code for
amputation of finger. With ICD-10, there are 32 codes that define which finger,
the level and the approach. An amputation of the tip of the small finger, for
example, requires minimal treatment and minimal risk to disability. However, an
amputation through the mid portion of the index finger requires removal of the
rest of the index and metacarpal and a reconstruction to convert it into a
functioning index finger. This type of amputation requires high surgical
involvement and is at risk for long term disability. With ICD-9, you cannot
tell the difference, but with ICD-10 the level of detail outlines the severity
and risk of the amputation.
The migration to ICD-10 will require changes in
documentation and coding practices… or it will simply become a burden to you with
little benefit.
Documentation Key Points to Consider
- Regardless of when the claim is submitted, ICD-10 codes are only to be used for service(s) provided on or after October 1, 2014.
- The code set has been expanded from five to seven positions. The codes use alphanumeric characters in all positions, not just the first position.
- The new code set increases the specifics of the reporting, allowing for more information to be communicated within the code. It also allows for future expansion and definitions.
- Most of the new concepts in ICD-10 coding are concepts that any physician is already documenting now. They understand the significance in understanding severity, risk and a variety of other important parameters related to proper health assessment and treatment.
- There are codes that are a combination of diagnoses and symptoms, so fewer codes may be needed to report or describe a condition.
- ICD-10 codes enable lateral reporting (right vs. left) reflecting which side of the body or limb is subject to evaluation. About 25,000 (36%) of the new codes are different only because they distinguish “right” vs. “left.” You can also report location such as medial, distal or proximal.
- Requirements are different for all specialties. For example, Ophthalmology codes have changed very little in scope, but codes for musculoskeletal systems have increased dramatically… over 50% of the ICD-10 codes are related to musculoskeletal conditions. Over 17,000 ICD-10 codes (about 25%) are related to fractures.
- There are some one-to-one mappings, but often there are one-to-many, many to one, many-to-many, or none at all. There is no clear mapping between ICD-9 and ICD-10.
- Transition to ICD-10 does not directly affect provider use of CPT or HCPCS codes.
Roles in Documentation
Criterions realizes and accepts the challenges of capturing
ICD-10 codes in your claims and EHR encounters and providing you with
proficiently trustworthy software that offers the ability to prepare and submit
claims reliably to your clearinghouse/payers, before, during and after this
transition.
Clinician
The role of the clinician is to document as accurately
as possible the nature of the patient conditions and services done to maintain
or improve those conditions.
Coding Professional
The role of the coding professional is to assure that
the coding is consistent with the documentation.
Business Manager
The role of the business manager is to assure that all
billing is accurately coded and supported by the documented facts.
Documentation Example
The following case highlights the increased specificity
required to code with ICD-10:
CHAPTER 2 - Challenges in Preparation
We realize the greater responsibilities and challenges
faced by our clients:
Understand the Magnitude
If you, the client, are using our Certified EHR, the
ICD-10 transition will be much easier. But, either way, you will need to have
an understanding of the scope of ICD-10, the implications and the impact its
transition will have on your office. We suggest downloading free ICD-10 fact
sheets and background information for your staff from the CMS website: www.cms.gov/ICD10
CMS Offers Important Guidance on Implementation
Look at implementation guides offered by CMS for
direction and assistance.
Learning to Code
You will need to learn to code each type of visit in
ICD-10 terms. We suggest securing ICD-10 Coding training from organizations such
as AAPC: http://www.aapc.com/icd-10/index.aspx
Criterions will not train on ICD-10 usage or train
anyone on appropriate ICD-10 billing codes.
The Unknown at This Time
At this time, there is no end-to-end or direct testing
available with payers… nobody knows which ICD-10 codes will be payable for a
routine CPT; and, no one knows to what degree or how strictly the payers will
enforce the most detailed ICD-10 coding processes. For example, no one knows at
this time if a payer may accept a comparatively simplistic translation, or may
require as many as seven ICD-10 codes for a procedure. A strict enforcement may
cause a confusion that Criterions cannot help with – we would need to refer you
to the payer for guidance.
The Paper “Superbill”
The TCMS paper Superbill feature is an instrument for
collecting data to be used for coding purposes. If you only use it for CPT
coding, you will not see a change; but, offices that utilize it and include
ICD-9 codes within the paper Superbill may or may not find it to be practical
under ICD-10 for your office. This may force a major change in the workflow or
methodology in offices that use a paper Superbill.
TCMS contains two on-screen Superbill-related features,
utilized by many of our clientele, known as the “Electronic Superbill” and the
“Electronic Superbill Queue.” The benefits of these two features include
reduced storage, ease of access, improved accuracy and reduced costs.
A handful of clients have been hesitant to convert from
the paper Superbill to one that is on screen but now may be the time to do it.
Making the change can be initially time-consuming; however, the benefits highly
outweigh the challenges. If your office is still using the paper Superbill and
including ICD-9 codes, you may find these features a necessary consideration
under ICD-10.
Claim Denials and Delays
Given the challenges in both the coding and
preparation, and the changes in processing rules imposed on the payers, all
providers may see a significant increase in denials. These denials may result
after the transition because of the increased coding detail. Payments and
approval of services may also be denied due to misinterpretations and errors in
translating ICD-9 to ICD-10.
There are also likely to be changes in how
authorizations are triggered or approved under ICD-10.
Conclusion of CHAPTER 2 - Challenges in Preparation
Learning to code and seeking out direction from CMS and
AAPC are keys to minimizing denials and delays to claims submissions. Because
there is no point-to-point testing with payers, the extent to an individual
payer’s coding requirements is an unknown challenge – making denials and delays
likely and preparation for these challenges essential.
Chapter 3 – ICD-10 Setup Preparation and Testing
In preparation for the impending change from ICD-9 to
ICD-10, Criterions has provided the ability to prepare your Setup screens for
ICD-10 and to test the transmission/acceptance processes with your
clearinghouse. Note that direct claim file submission testing with payers is
not yet available and can only be performed with clearinghouses at this time.
COST OF AUTOMATION (TCMS Clients only) –
The
“automated syncing” (Step 2a below) and “automated mapping” search feature
processes (Step 2b below) utilize an outside service that is purchased by your
office for $35 per month/per provider.
Without
this service, the processes can still be performed, at no cost, by manually finding
the ICD-9 to ICD-10 code and by searching for ICD10 codes from any other
outside source and manually adding them to TCMS going forward.
EHR
Clients will not need this feature.
Setup Preparation
The following is a detailed 4-step process intended to
help you prepare and send a test claim file to your clearinghouse:
Step #1 – Select the New Practice Default
There is a new Practice Default setting in Criterions
that when selected, will signal TCMS to generate ICD-10 output and results. If
this setting is unchecked, ICD-10 features will not be activated. The setting is
the bottom-most choice in the “Claims” section, and is labeled “Use ICD10 Codes
– Effective October 1st 2014.”
Step #2 – Sync Your Current ICD-9 Codes to ICD-10
Codes
Sync and or map your current ICD-9 codes to ICD-10
codes. “Syncing” is automated while “mapping” is a manual selection
process. This is a two-step process (Steps
2a and 2b below) which can generate a majority of corresponding ICD-10 codes for
your current ICD-9 codes:
Step 2a
- To Sync the codes (automatically):
Go to the Diagnosis Code
Setup screen and find the new button labeled “Sync ICD10” (as shown below). By
clicking on this button, TCMS will automatically sync your current ICD-9 codes
to the new corresponding ICD-10 codes. Note that TCMS may not be able to sync
all of your ICD-9 codes to ICD-10 codes because not all codes have a one-to-one
relation.
After syncing
automatically, many of your ICD-9 codes may now have a corresponding ICD-10
code linked to it. There are two new columns in the Diagnosis Setup screen that
will display the mapped ICD-10 codes:
You may also see that some
ICD-9 codes did not return a one-to-one translation in ICD-10. As a result,
there will be a need for your office to fill in the gaps caused by either
missing ICD-10 codes or having too many ICD-10 codes to choose from. These are
the codes that you can now “map” (manually):
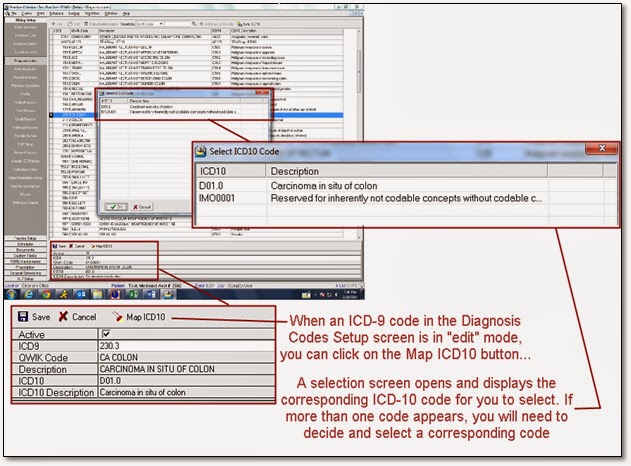
Step 2b
- To Map the codes (manually):
Go to the Diagnosis Code
Setup screen and double-click on an ICD-9 code that did not return a
corresponding ICD-10 code after syncing. This will put the ICD-9 code in edit
mode, and will display:
1- A new
button labeled “MapICD10”
2- A new
storage field for the ICD-10 code
3- A
new storage field for the ICD-10 description
Click on the option “Map
ICD10” button and TCMS will utilize a database that can provide ICD-10
translations for the ICD-9 code. The display will contain several ICD-10 code
translations for the ICD-9 code. You will need to select the most appropriately
corresponding ICD-10 code to enter them into the two new storage fields.
You may (or may not) need
to create new entries for unmapped ICD10 codes.
The mapping process may
also not return an ICD-10 response if there isn’t an available translation for
the ICD-9 code.
You will want to use the
most specific ICD-10 code for routine visits. Unfortunately, not all ICD-9
codes have a direct/single/one-to-one translation to ICD-10. That means mapping
ICD-9 to the ICD-10 code may not be enough if the mapped ICD-10 code is not
specific enough.
Step #3 – Setup a Carrier for ICD-10 Submission
The Insurance Carrier Setup screen contains all of the
insurance carriers used by your practice. Although a carrier’s readiness for
ICD-10 is expected as of Oct 1, the software allows the possibility of carrier
exceptions. Each carrier’s edit screen contains a new checkbox that, when
checked, will identify it as a carrier that you are ready to submit claims
containing the new ICD-10 codes.
Step #4 – Enter an ICD-10 Start Date
The Practice Information screen has a new field at the
bottom in which you can enter your practice’s ICD-10 Start Date. The date
entered here is the earliest service date for which a file can contain claims
with ICD-10 codes.
The date entered here will eventually be Oct 1, 2014,
but you may want to use an earlier date for Clearinghouse testing purposes as
discussed later in this document.
Diagnosis Analysis Report
TCMS offers a preparatory report that will identify your
most utilized ICD-9 codes within a service date span and their corresponding
ICD10 code. This report will confirm that you have mapped your most common
ICD-9 codes to ICD-10:
Testing
With a Clearinghouse
To send a file for testing with your clearinghouse, all
of the four preparation steps noted above must be performed.
TCMS will include the ICD-10 code(s) on claims if:
- The Practice Default is activated/selected (Step 1), and…
- The ICD-10 code exists and synced to the ICD-9 already on the claim (Step 2), and…
- The carrier is set up for ICD-10 submission (Step 3), and…
- The claim’s service date is after the ICD-10 Start Date (Step 4).
The clearinghouse will respond with a “999” confirmation that the file is acceptable but will not forward the claims to the payers for further adjudication or testing. An acceptable response confirms your ability to submit ICD-10 coded claims to the clearinghouse.
YOU CAN PERFORM ALL PREPATORY WORK WITHOUT AFFECTING
YOUR CURRENT CLAIM ENTRIES OR SUBMISSIONS.
DO NOT WAIT FOR THE LAST MINUTE.